Running a successful healthcare practice means mastering the delicate balance between patient care and financial health. Revenue cycle management sits at the heart of this challenge, determining how efficiently your practice converts services into cash flow.
Whether you're managing a single practice or overseeing multiple locations, optimizing your revenue cycle can mean the difference between thriving and merely surviving in today's complex healthcare landscape.
Fundamentals of effective revenue cycle management
Revenue cycle management (RCM) encompasses every financial touchpoint in the patient journey. It begins when a patient schedules an appointment and ends when the account balance is resolved through reconciliation.
For healthcare organizations, this process involves multiple complex steps that must work together seamlessly. Understanding these fundamentals can help you identify where improvements could have the greatest impact on your practice's financial health. Each stage presents opportunities to optimize processes and reduce the time between service delivery and payment.

Key steps in the revenue cycle management process
A well-functioning revenue cycle moves through several stages, each building on the one before. Improving revenue cycle management performance requires a well managed revenue cycle at every stage of the journey.
Patient scheduling and registration
The cycle begins when patients schedule appointments. Collecting accurate personal and insurance information can help prevent issues downstream, but the moment personally identifiable information (PII) is entered, HIPAA comes into play, requiring careful attention to data storage and transfer.
Insurance verification and authorization
Confirming coverage and obtaining necessary pre-authorizations can help ensure that services will be reimbursed and patients will fully understand their financial responsibility.
Service delivery and documentation
The detailed documentation required for patient care is equally important in supporting accurate coding and billing. Insurance justifications need to be supported by written records.
Charge capture and coding
Translating services into billable codes requires accurate, up-to-date knowledge of coding guidelines and payer requirements. A quality assurance (QA) check here can go a long way toward avoiding errors.
Claim submission
Clean claims submitted promptly to the correct payer accelerate the payment timeline. This means they're accurate, complete, timely, and compliant with the payer's rules, regulations, and coding guidelines.
Payment posting and reconciliation
Applying the right payments to the right bills and identifying any variances will help keep your accounts current while highlighting the need to follow up with any reminders or collections.
Denial management and appeals
Responding quickly to denials by appealing the decision with appropriate documentation can help protect justifiable revenue that might otherwise be lost.
Patient collections
Following up on patient balances with clear communication and convenient, flexible payment options completes the revenue cycle.
What is the biggest obstacle to good revenue cycle management?
One of the toughest aspects of revenue cycle management is maintaining a timely collections rate. This challenge has only intensified as patient financial responsibility continues to grow.
With the rise in high-deductible health plans, patients are increasingly responsible for a larger portion of their healthcare costs. This shift creates collection challenges that many practices aren't equipped to handle effectively.
Ideally, the medical provider will receive timely patient payments for all doctor services, including appointments, visits, and therapeutic procedures. But when payments are delayed or denied, cash flow suffers, and administrative costs can skyrocket.
The sheer complexity of insurance requirements adds another layer of difficulty. Payer requirements change often and vary widely among the hundreds of providers operating in the U.S. Keeping up with these constant changes while maintaining efficient operations can be difficult for healthcare organizations of any size.
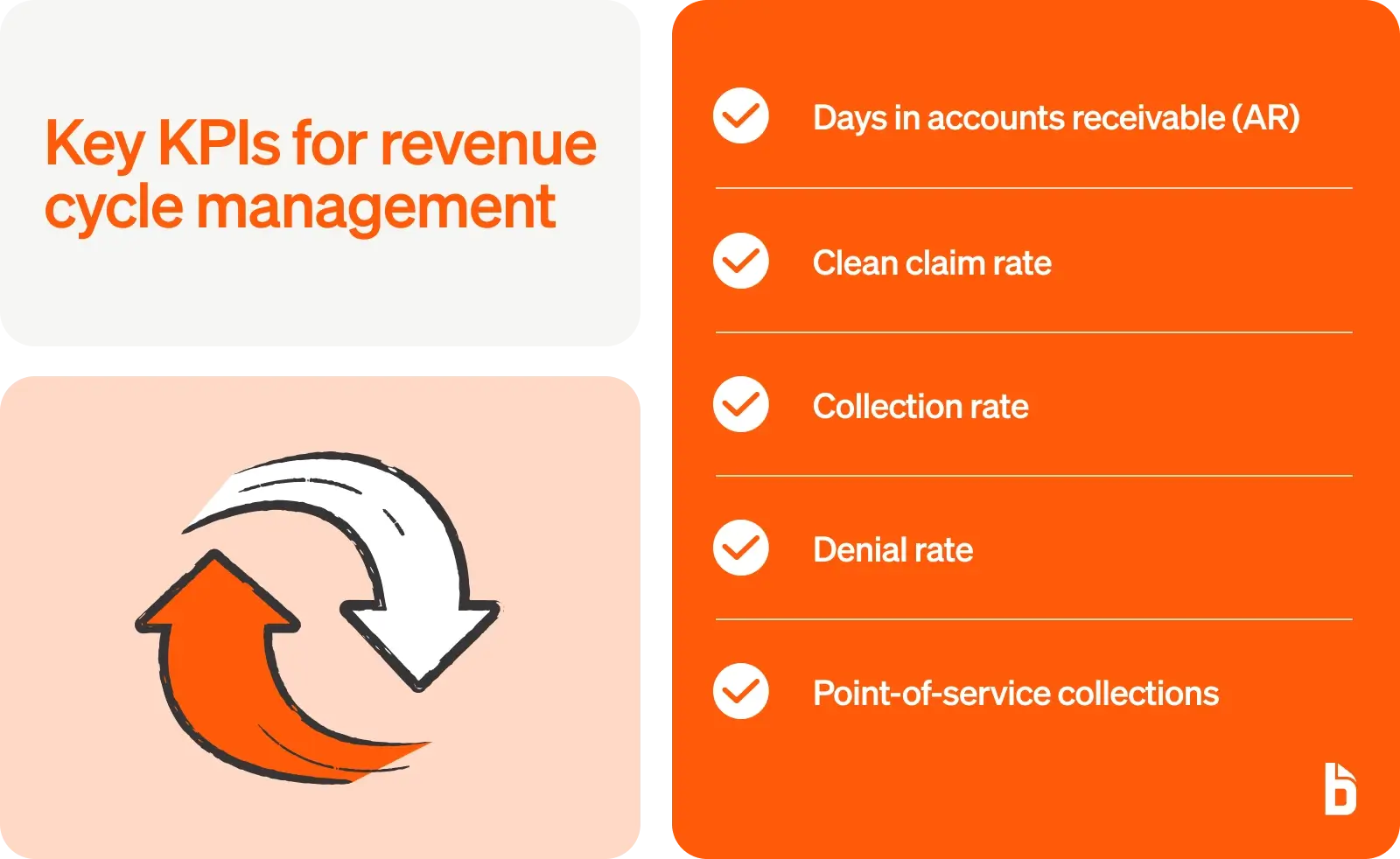
What are KPIs for revenue cycle management?
Tracking the right metrics can help healthcare organizations understand where their revenue cycle performance needs improvement. These key performance indicators provide actionable insights that can transform your financial operations.
Days in accounts receivable (AR)
This component can help evaluate your revenue collection processes, tracking the length of time it takes to collect payment for each invoice. Lower numbers indicate faster collections and better cash flow.
The American Academy of Family Physicians (AAFP) recommends that Days in AR should stay below 50, with 30 to 40 days being preferable. Some high-performing practices may achieve even better results through strategic improvements.
Clean claim rate
Your clean claim rate measures the percentage of claims accepted on first submission. This benchmark measures "clean billing." It tracks claim denials and related errors, and it assists with forming an action plan to fix problems when necessary.
Higher clean claim rates mean faster payments and less time spent on rework. Top-performing organizations try to achieve clean claim rates above 95%.
Collection rate
The collection rate shows what percentage of collectible revenue you actually receive. This metric helps identify gaps in your billing and collection processes.
A strong collection rate indicates effective patient communication, accurate billing, and efficient follow-up processes. Industry benchmarks vary, but successful practices aim for collection rates above 96%.
Denial rate
Denials occur when a payer refuses to reimburse the healthcare provider for a particular service. Tracking denial rates by payer and reason helps identify systemic issues.
Beyond denied claims, healthcare practices face significant challenges to their financial health due to the pace at which even accepted claims are paid. According to data from over 1,800 hospitals and 200,000 physicians analyzed by Crowe Revenue Cycle Analytics, almost one in three inpatient claims submitted by providers to commercial insurers in the first quarter of 2023 went unpaid for more than three months.
Point-of-service collections
This data reports copayment collection at the time service is provided. Strong POS collections reduce back-end collection costs and improve overall revenue cycle efficiency. Practices that excel at point-of-service collections can see significant improvements in their overall financial performance.
How can revenue cycle management be improved?
Improving your revenue cycle requires a systematic approach that addresses revenue cycle challenges at each stage of the process. These proven strategies can help enhance your financial stability.
Strengthen patient registration and verification
Accurate patient information forms the foundation of successful revenue cycle management. Capturing patient data fully and without errors increases the likelihood you'll file claims correctly the first time.
Start by implementing thorough verification processes at registration. Train staff to collect complete personal and insurance information, verifying coverage details before services are rendered.
Consider automating insurance eligibility checks to reduce manual errors. Real-time verification can identify coverage issues before they become collection problems.
Optimize coding and documentation
Coding errors can look like medical errors, leading to higher rates of claim denials. Conversely, investing in proper training and quality control processes can pay dividends through improved claim acceptance rates.
Regular coding audits help identify error patterns early, before they become systemic issues. Create feedback loops between coders and providers to ensure you have proper documentation to support the codes being submitted.
Stay current with coding updates and payer-specific requirements. Coders must stay on top of ever-changing guidelines for specialty areas, understanding how treatments should be reflected in medical billing.
Implement proactive denial management
Rather than simply reacting to denials, successful organizations develop proactive strategies to prevent them. Analyze denial patterns to identify root causes and implement targeted improvements.
Proactive AR management identifies reasons for claim denials and corrects issues before submission, increasing the first-pass claim acceptance rate and reducing rework costs.
Create a dedicated denial management team or assign clear responsibilities for denial follow-up. Quick response times can improve your chances of successful appeals.
Enhance patient financial communication
Clear communication about financial responsibilities tends to improve both collection rates and patient satisfaction. Practices can reduce delinquent payments by setting clear financial expectations before scheduled visits.
Provide cost estimates before services when possible, explaining insurance coverage and patient responsibilities in plain language that patients can understand.
For even better results, offer multiple payment options to accommodate different patient preferences and financial situations. Providing multiple convenient payment options, like online portals or payment plans, enhances patient satisfaction and facilitates timely payments.
Build a skilled revenue cycle team
Your revenue cycle is only as strong as the people managing it. Medicare and Medicaid claims are complex and require people who are billing experts with knowledge of their ever-changing rules and regulations.
Invest in ongoing training to keep staff current with regulatory changes and best practices. Cross-training creates flexibility and ensures coverage during absences.
When clinical and financial teams collaborate smoothly, financial performance tends to improve. Healthcare revenue cycle management teams should have weekly meetings to discuss AR reports, work together to resolve issues, and strive to submit claims for payment as soon as possible.
Focus on high-value accounts
Not all accounts receivable require the same level of attention. Data-driven strategies that prioritize collections from high-value accounts can help maximize revenue recovery.
To achieve this objective, develop workflows that prioritize accounts based on value and age. This helps your team focus efforts where they can have the greatest financial impact, but remember to consider the total relationship value when making collection decisions. Sometimes, flexibility with a high-value patient may protect long-term revenue.
Monitor and optimize continuously
Revenue cycle improvement isn't a one-time project—it requires ongoing attention and refinement. Run weekly AR reports to track older bills.
Regular performance reviews help identify emerging issues before they impact cash flow. Compare your metrics to industry benchmarks to understand where you have the most opportunity for improvement.
Create accountability by assigning ownership of specific metrics to team members, and celebrate improvements to maintain momentum and engagement.
Leverage technology and automation
These strategies can represent a significant amount of work, but modern technology can transform revenue cycle efficiency with a lot less effort. Automating routine tasks allows revenue cycle specialists to focus on more complex aspects of RCM.
Automated payment reminders reduce the administrative burden of collections while improving payment rates. Electronic payment options make it easier for patients to pay their bills quickly. And integration between systems can eliminate duplicate data entry and reduce errors.
Look for solutions that connect seamlessly with your existing practice management software.
How BILL Accounts Receivable can support revenue cycle management
BILL Accounts Receivable transforms healthcare revenue cycles by automating the most time-consuming aspects of billing and collections. The platform addresses the specific challenges healthcare organizations face in managing their revenue cycle.
Faster invoicing and payments
AI and automation can reshape business priorities. BILL leverages these technologies to accelerate your payment cycle, automating invoice creation and delivery to help bills reach patients quickly and accurately.
Get paid 2 times faster, and save up to 50% of time spent on accounts payable. Multiple payment options give patients flexibility while automated payment processing speeds up cash application.
Plus, digital payment capabilities mean you can accept payments 24/7, improving convenience for your patients while accelerating your collections.
Cash flow visibility
Understanding your cash position is critical for healthcare financial management. BILL provides real-time visibility into outstanding invoices and expected payments.
Get the complete picture of money coming in and out of your business to make more informed decisions, faster. Dashboard views show aging receivables, payment trends, and collection performance at a glance.
This visibility helps you identify potential cash flow issues early and take corrective action before they impact operations.
Automation and workflow efficiency
Manual processes slow down collections and increase errors. Easily nudge customers by setting up automated reminders that go out at optimal times to encourage payment.
BILL can also help with recurring invoices and overdue reminders. These automated touchpoints maintain consistent communication without adding to staff workload. The platform's intelligent workflows route exceptions to the right team members while handling routine tasks automatically.
Improved accuracy
Billing errors damage patient relationships and delay payments. BILL's automation reduces manual data entry and the errors that come with it.
Sync customers, invoices, accounts, classes, and more—two ways. This integration ensures your billing data stays accurate and up to date across all systems.
Automated reconciliation can catch discrepancies quickly, for faster resolution of payment issues.
Audit trail and compliance
Healthcare organizations need to maintain detailed records for compliance and reporting. BILL automatically creates comprehensive audit trails for every transaction.
The platform offers a suite of features designed to eliminate paper-based processes, making it easier to maintain HIPAA-compliant documentation. These electronic health records simplify audits and provide the documentation needed for regulatory compliance and financial reporting.
Transform your healthcare revenue cycle with BILL
Improving revenue cycle management requires the right combination of processes, people, and technology. BILL Accounts Receivable provides the automation and insights healthcare organizations need to optimize their financial performance.
The platform helps practices like yours reduce days in accounts receivable, improve collection rates, and free up staff to focus on patient care. See how practices across the healthcare industry are transforming their revenue cycles with BILL.
"BILL allows us to function in a multi-location space by having one software for our accounts. It's seamless and efficient for one staff accountant to bounce between locations and update the latest AP information across multiple practices." — Lightwave Dental
"Growing as fast as we did would have been really difficult without BILL." — Guardian Dentistry Partners